The program trained 580 community health workers — a global average of 70% of whom are women — and reached over 22,000 people, resulting in decreased rates of cardiovascular events and glucose levels, as well as noncommunicable disease (NCD) service utilization.
Background
Dealing with chronic diseases during crisis
In the aftermath of crisis, many people struggle with managing, or preventing, chronic diseases such as diabetes and cardiovascular disease. This is only expected to get worse as disasters — natural and human-made — increase, most acutely for those least equipped. Despite a significant need for uninterrupted care, chronic diseases often don’t receive enough attention in these emergency settings.
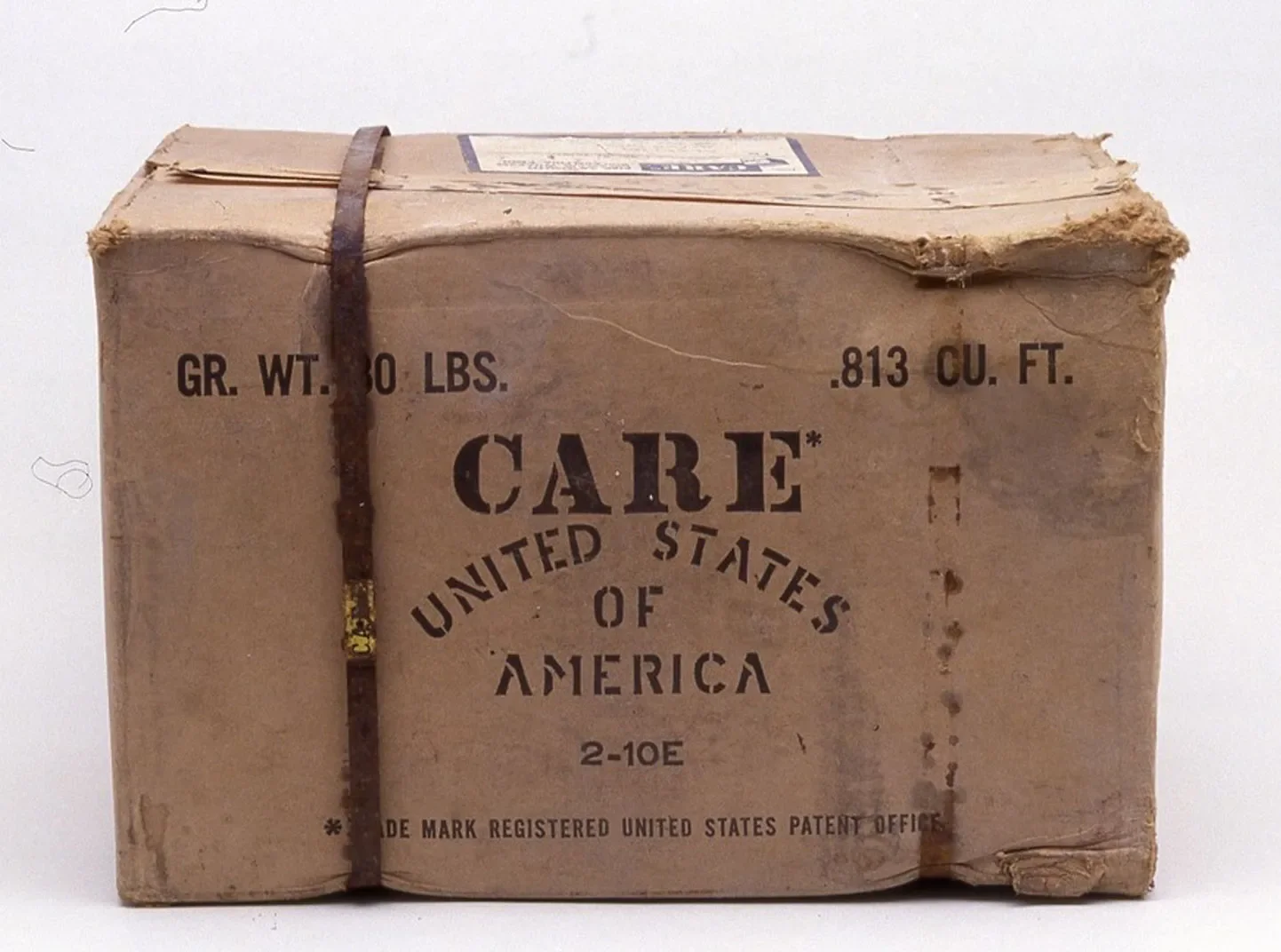
Future Well in Crisis was a four-year program (2019-2023) that built on CARE’s longstanding partnership with the global healthcare company Abbott and its foundation, the Abbott Fund. The program amplified the success of previous humanitarian investments, scaled proven approaches, and explored new opportunities to prevent, control, and treat chronic diseases like diabetes.
The program aligns with CARE’s Right to Health strategy, as well as the She Heals the World initiative, and contributed to ensuring that by 2030 over 1 million female frontline Community Health Workers (CHWs) are equally trained, equipped, and paid to do their lifesaving work. The program increased equal access to healthcare at the last mile and ensured that 50 million people were able to realize their right to health.
Program activity
Helping internally displaced people living with noncommunicable diseases
The four-year program focused on helping internally displaced people living with diabetes, hypertension, and/or obesity in post-conflict Marawi, Philippines. Baseline screening found that three out of four adults (75%) had never had their glucose tested, and 16% of adults were either diabetic or pre-diabetic. Of those identified as diabetic, more than half (59%) had not been previously diagnosed.
Our work focused on three things:
- Screening to identify people with NCDs and those at risk of developing them
- Providing health education, counseling, monitoring, and referral services to NCD patients
- Building local capacity to deliver NCD services and partnering with the local health system to ensure prioritization of NCDs in displaced communities
Key elements of the program included:
- Training and advocating for CHWs
- Collecting data on diabetes rates and sharing with key government stakeholder
- Establishing and running NCD Corners with CHWs in 15 municipalities
- Establishing and running NCD clubs
To support the partnership, the Abbott Fund provided $1.4 million in funding, and Abbott donated its technologies to advance testing and care, including rapid testing technology and glucose monitoring systems for diabetes management. Abbott experts also provided training on the use of these technologies for local healthcare providers and volunteers.
Results
An effective model for addressing NCDs in emergencies
These efforts led to a diabetes diagnosis for 2,800 individuals and a 20% increase in NCD service utilization within the government health system. They also resulted in a budget increase for diabetes care and CHWs, as well as greater awareness of the need to prevent and control hypertension, diabetes, and obesity in emergency settings.
After receiving specific support, including monitoring and counseling, more than half (51%) of diabetic and pre-diabetic patients saw a decrease in their fasting blood glucose levels since the baseline, and 46% saw a decrease in their average blood glucose (HbA1c) levels, which is an indicator of better glucose control and lower risk of complications.
After four years, CARE handed over the program to the local government in Marawi. This led to more government investment in NCDs, such as funds and staff. The program was also replicated with private funds in Arteche and Jipapad.
This project provides an effective model for addressing NCDs in emergencies and can be replicated in other parts of the Philippines and potentially globally. The team has used events and publications to raise awareness of and encourage investment in preventing, controlling, and treating diabetes in emergency settings.